Search Knowledge Base by Keyword
Abnormal Changes in BMD of the Hip
Submitted By: Steven Petak MD JD MACE FACP Associate Clinical Professor Weill-Cornell Medical College Division Head Endocrinology and Chief of Endocrinology, Houston Methodist Hospital
Patient History:
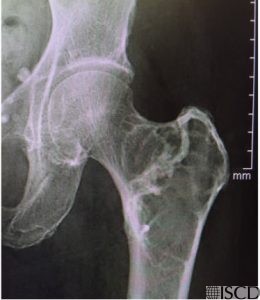
An 85 year old woman with mild hip pain – long standing – for routine DXA. Discordance changes noted at the hips, with increased BMD at the left hip (Figure 1) compared to the right hip. (Image not shown). (Figure 2).
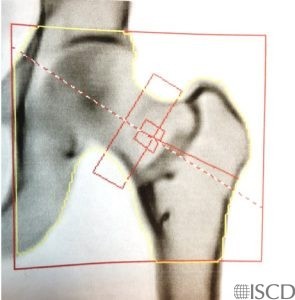
Figure 1: DXA image of left hip Right hip image was unremarkable (not shown.)
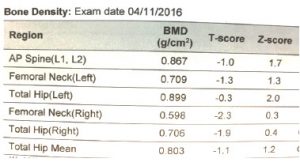
Figure 2: DXA scan results. Degenerative changes at the spine limited assessment to only the upper two vertebral bodies.
Questions:
- Are there abnormalities to the appearance, positioning, or analysis of the left hip?
- What possible etiologies can explain the left hip findings?
- Answers
- There is a curvilinear area of increased density at the base of the femoral neck. The patient is properly positioned and ROI placement is appropriate.
- Images by DXA are not of sufficient resolution to identify or differentiate disease processes. Sometimes, visual comparisons to previous studies can often help identify that morphologic changes have occurred, and are a sufficient reason to recommend higher order diagnostic testing. Plain radiographs were ordered to assess the atypical DXA image (Supporting images below)
- DiscussionFrom the radiologic standpoint, the differential diagnosis for this well-defined lucent lesion with sclerotic margins, lacing mineralized matrix located in the neck, intertrochanteric and subtrochanteric region of this left femur includes intra-osseous lipoma, fibrous dysplasia, and liposclerosing myxofibrous tumor (LSMFT). Plain films and additional work-up led to a final diagnosis of LSMFT. This type lesion appears to be confined to the intertrochanteric region of the hip, and the lesion tends to be well-defined with a sclerotic rim, with little or no disruption of the endosteal bone contours. Many are associated with underlying fibrous dysplasia on biopsy. (1-2) It may well be that LSMFT is a variant of fibrous dysplasia. (3)
Supporting Images:
Supporting Image 1: AP radiograph of left hip.
Supporting Image 2: Lateral x-ray of left hip.
Key Teaching Point:
- While DXA is not typically able to make a differential diagnosis, the disclaimer “Image not for diagnostic use” is not meant to discard the image. To borrow a phrase from another unrelated but similarly serious issue, “If you see something, say something” is good advice for physicians who interpret bone densitometry exams.
- Unexplained discordance in BMD values warrant more careful visual examination of the underlying images from which they were calculated. Once technical errors in acquisition (external artifacts, scan mode, anatomic positioning) and analysis (incorrect bone mapping, regions of interest size and placement) have been excluded, and external causes such as relative disuse have been considered, higher order imaging should be considered appropriate, if not already done.
- Reference database derived values (i.e. T-scores or Z-scores, FRAX) assume the underlying anatomy from which they are calculated is normal. In this case, left hip results or any mean values from bilateral hip measurements should not be used for diagnosis or fracture risk assessment.
References:
- Kransdorf MJ, Murphey MD Sweet DE. . Liposclerosing Myxofibrous Tumor: A Radiologic-Pathologic-Distinct Fibro-osseous Lesion of Bone with a Marked Predilection for the Intertrochanteric Region of the Femur. Radiology. 1999;212(3):639-8.
- Dattilo J, McCarthy EF. Liposclerosing myxofibrous tumor (LSMFT), a study of 33 patients: should it be a distinct entity? Iowa Orthop J. 2012;32:35-9.
- Heim-Hall JM1, Williams RP. Liposclerosing myxofibrous tumour: a traumatized variant of fibrous dysplasia? Report of four cases and review of the literature. Histopathology. 2004 Oct;45(4):369-76